BRASH syndrome
Homepage: EMNote.org
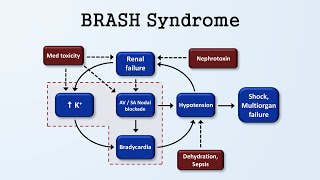
BRASH syndrome is a constellation of symptoms that includes bradycardia, renal failure, atrioventricular (AV) nodal blockade, shock, and hyperkalemia.
The syndrome is caused by medicationinduced AV nodal blockade, such as betablockers or calcium channel blockers, leading to bradycardia, poor tissue perfusion with decreased cardiac output, shock, renal failure, and subsequent hyperkalemia, which further exacerbates bradycardia.
In this blog post, we will discuss the pathophysiology, clinical features, and management of BRASH syndrome.
Pathophysiology:
Population at risk of developing BRASH syndrome are elderly patients with vulnerable renal function who are prone to volume depletion and, at the same time, taking AV nodal blocking agents such as betablockers.
BRASH syndrome is a vicious cycle in the setting of medications, hyperkalemia, and renal failure.
Renal failure causes hyperkalemia.
Hyperkalemia synergizes with AV node blockers to cause bradycardia and hypoperfusion.
Hypoperfusion, in turn, causes worsening of the renal failure.
The inciting factor of BRASH syndrome is generally considered to be something that prompts acute kidney injury, often hypovolemia of some sort. Rather than AV nodal blocker overdose or severe hyperkalemia causing conduction problems, the combination of AV nodal blocker use and moderate hyperkalemia has a synergistic effect on cardiac conduction, causing further bradycardia that results in renal failure and shock.
Clinical Features:
Patients with BRASH syndrome may present with heterogeneous, nonspecific symptoms, including generalized weakness, dizziness, and syncope.
While it is commonly precipitated by betablockers or calcium channel blockers, other agents such as amiodarone, digoxin, and octreotide are also associated with the onset of the disease.
Management:
Treatment of BRASH syndrome is supportive, but most effective when the syndrome is promptly recognized and all symptoms and signs are simultaneously managed.
Physicians should be familiar with its existence in order to avoid diagnostic and treatment delay.
Clinicians should aim to treat hyperkalemia, bradycardia, hypovolemia, and renal hypoperfusion, simultaneously.
Shock is managed with intravenous fluid resuscitation.
Epinephrine infusion may be needed to treat severe bradycardia.
Hyperkalemia is managed with intravenous calcium, intracellular potassiumshifting medications, and loop diuretics.
Bradycardia is managed with intravenous calcium and epinephrine (or isoproterenol).
Cardiac pacing is rarely needed.
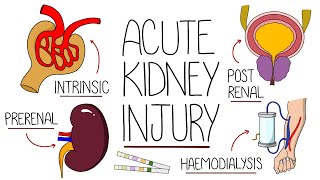
Renal failure is managed with intravenous rehydration. Severe cases of renal failure may require hemodialysis.
Pitfalls:
The most common error in managing BRASH syndrome is fixating on a single component of the syndrome, for example, hyperkalemia, and focusing solely on management of that problem, for example, emergent dialysis; meanwhile, other aspects of the syndrome are overlooked, for example, the patient might remain underresuscitated, bradycardic, and malperfused.
Take Home Message:
In conclusion, BRASH syndrome is a relatively new clinical entity that includes bradycardia, renal failure, AV nodal blockade, shock, and hyperkalemia.
It is caused by medicationinduced AV nodal blockade leading to bradycardia, shock, renal failure, and subsequent hyperkalemia, which further exacerbates bradycardia.
BRASH syndrome may present with heterogeneous, nonspecific symptoms, including generalized weakness, dizziness, and syncope, which could be easily misdiagnosed if clinicians are unaware of the association between AV nodal blocking agents and the possible consequences of bradycardia, renal injury, and shock.
Treatment is supportive, but most effective when the syndrome is recognized and all symptoms and signs are managed simultaneously.