Cervical Myelopathy - Everything You Need To Know - Dr. Nabil Ebraheim
Dr. Ebraheim’s educational animated video describes the condition of cervical spine myelopathy.
Follow me on twitter:
https://twitter.com/#!/DrEbraheim_UTMC
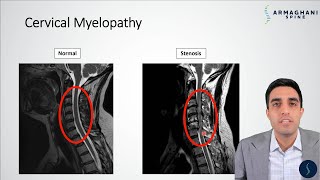
Cervical Myelopathy
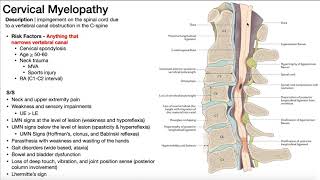
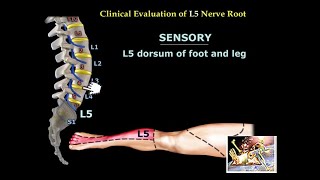
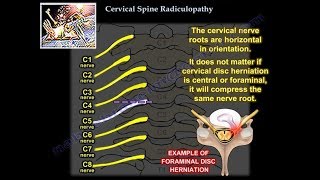
Cervical spine myelopathy can occur due to compression of the cervical spinal cord at the cervical spine level. Cervical spine myelopathy is caused by spondylosis, cervical stenosis, cervical disc herniation, tumors, or ossification of the posterior longitudinal ligament (OPLL). OPLL can occur more in people of Asian ancestry. C4C6 is the most frequently involved level and can be seen on CT scans. Exacerbation of symptoms followed by a long period of static or deteriorating function (stepwise pattern). 75% of patients will have long periods of stable neurologic function, which may be for years. In the majority of patients, the condition deteriorates between quiescent streaks. The condition does not improve without surgery. Pain is absent or poorly defined with vague sensory and motor changes. The patient will have progressive gait and balance disturbance. Broad based ataxic gait and unsteady gait. There will also be intrinsic muscle weakness with difficulty in buttoning the shirt and performing fine manual activities (weakness of grip strength). Poor hand fine motor function and dexterity occurs early. Pathologic long tract signs will be seen consisting of ankle clonus. Clonus sign is a nonvoluntary sustained movement of the ankle muscles with firm, passive, continuous stretch. Pathologic long tract signs will be seen consisting of positive Hoffman’s sign in about 80% of patients. The Hoffman’s sign is done by flicking the nail of the middle or ring finger to produce flexion of the index finger to the thumb. Pathologic long tract signs will be seen consisting of bilateral outgoing toes by a positive Babinski reflex.The Nurick classification deals with walking ability and gait. It ranges from normal to wheelchair bound. When you have cervical myelopathy, you need to get an MRI. MRI is the best study, it shows the compression and the changes in the spinal cord (look for bright signal in T2 MRI). In patients with low back pain and gait disturbance, look into the spinal cord, especially into the cervical spine. Some of these patients will have lumbar spinal stenosis and they come to the doctor with an MRI of the lumbar spine that shows lumbar stenosis, but the patient also has gait disturbance. The patient examination may be confusing because they will come to the doctor with low back pain and a positive MRI for lumbar spinal stenosis. Lumbar stenosis and cervical spine stenosis can coexist together in about 20% of the patients. Cervical myelopathy can have a differential diagnosis of amyotrophic lateral sclerosis (ALS), syrngomyelia, spinal cord tumor, or multiple sclerosis. ALS is a motor neuron disease affecting both upper and lower extremities with no sensory changes, and will lead to progressive weakness, muscle atrophy fasciculation and spasticity, in addition to dysphagia and respiratory compromise. In multiple sclerosis, the patient will have cranial nerve involvement, and the jaw jerk test is positive. Cervical myelopathy is progressive, and it rarely improves with nonoperative modalities. Decompression and fusion in case the symptoms are progressive or severe. Patients with rheumatoid arthritis are going to surgery for symptomatic cervical myelopathy. The neurological recovery after decompression is best predicted by presurgical posterior atlantodens interval exceeding 13 mm. with more than 10 mm space for the spinal cord, the patient will usually have improved neurological function. The patient will die earlier if the patient does not have surgery. Surgery is usually done anteriorly with decompression and fusion. One to two level disease, do anterior cervical decompression and fusion, especially with a fixed cervical kyphosis to more than 10o. Multilevel involvement of three or more disc spaces is easier to be managed by posterior approach if there is no fixed kyphosis. Lateral xray will show if there is any kyphotic alignment. You will do multilevel posterior decompression and fusion for multiple levels of involvement. Posterior approach has a higher incidence of would infection. You should not do posterior fusion if there is a cervical kyphosis. The residual kyphotic posture of the cervical spine will result in persistent spinal cord compression. For fixed kyphosis more than 10 degrees, you will need to go anteriorly (don’t go posteriorly if more than 10 degrees kyphosis exists. For multilevel cervical spondylitic myelopathy, the most common adverse postoperative complication is loss of range of motion up to 50%. Laminoplasty is used instead of Laminectomy to prevent progressive kyphosis. Laminoplasty is done by decompression of the cervical spine by widening of the spinal canal. The patient may get nerve root palsy (C5 nerve root is usually the most common involved nerve root).