Diagnosing Sacroiliac Joint Pain Is Challenging - Everything You Need To Know - Dr. Nabil Ebraheim
Dr. Ebraheim’s educational animated video describes the condition of SI joint pain Why is the diagnosis of SI joint pain challenging?
Follow me on twitter:
https://twitter.com/#!/DrEbraheim_UTMC
Find me on Instagram @OrthoInitiative
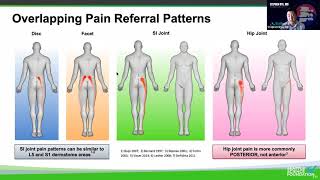
We all know that low back pain is very common. The sacroiliac (SI) joint is a major source of low back pain because it is responsible for approximately 22% of all low back pain and about 40% in patients with lower spine fusion. The problem is that the pain originating from the SI joint is usually attributed to other sources such as the spine and the hip. Patients with low back pain spend months or years in treatment without correct diagnosis. Patient with chronic low back pain and this patient is not improving with treatment, it is important to look at the SI joint as the source of the low back pain. So why is diagnosing the SI joint unique and why is there confusion about diagnosing SI joint pain? Why will the patients go to see multiple health care providers and get multiple diagnosis with many images and MRIs? The MRIs alone could give false positives about the intervertebral disc condition. And why are we missing the real pain generator, which is the SI joint. The truth is that the SI joint does not have a known cause for the pain. Diagnosing the SI joint pain is challenging. There is no radiological study or a clinical exam that can give us a reliable diagnosis. The SI joint is less recognized as a cause of low back pain. This is not something the MRI, the xray or the CT scan can show clearly. Up to 25% of asymptomatic patients over the age of 50 years old will show abnormal SI joints in the xray. It is known that the articular surface of the Si joint changes with age. The synovial surface begins to degenerate by the age of 50 and closure of the SI joint is common in men after the age of 50. When there is a previous lumbar fusion check the xrays carefully. Make sure that the hardware is stable. There is a wide variability in the clinical presentation from localized pain to tenderness around the SI joint, to radiating pain that looks like sciatica. The Si joint pain overlaps with spine pain and hip pain. The Si joint pain can be similar to facet joint pain, sciatica, disc herniation, or discogenic pain. SI joint pain can mimic sciatica, mimicking disc herniation. The SI joint must be part of low back pain evaluation. Make sure you have a high index of suspicion for every patient with low back pain. Make sure that the patient’s description and location of the symptoms is clear to you. Ask the patient “where is the maximum area of pain?” The Fortin finger test is confirmed when the patient points to the area of the pain by the finger just medial and inferior to the PSIS. Where does it hurt? If the patient points with the finger below the L5 level, then this is the Fortin finger test and it is suggestive of SI joint pain. Versus if the patient places a hand above the L5 level. Then this is probably low back pain due to spine causes especially if the patient’s pain is in the midline. Placement of a finger describes the pain over the painful area, is to the side, at, or below the PSIS. The pain is usually below L5 level in majority of cases. After we find the location of the pain by the Fortin test, tell the patient we are going to do examinations to provoke the symptoms because we are going to try to find the cause of the pain. Ask patient to tell you if it is the same pain or different pain. The whole idea is that shear of the SI joint reproduces the pain. With three or more positive provocative tests, we will need further investigation to confirm the diagnosis. The compression test and the thigh thrust test are considered to be the most valuable tests. Recommend the injection when the patient has a positive history, positive Fortin finger test, positive provocative tests, negative lumbar and hip examination and negative xrays. Use the injection to confirm the history and the physical examination. Use ultrasound or fluoroscopy for the injection. Some problems with injection. Two thirds of patients have 50% pain reduction for about six weeks. Value of injection is lower in patients with spine fusion. Do not inject more than three times within six months or four times in one year. If you have 75% pain improvement is a positive test which means that SI joint is the pain generator. If you have 5075% improvement, then this is an equivocal test and then you repeat the injection because the patient may have multiple pain generators. If you have minimal or no response, then this is a negative test and the SI joint is probably not the source of the pain. Treatment of SI joint dysfunction is usually conservative without surgery. Surgery is done by Si joint fusion leads to symptomatic improvement when the SI joint is the primary pain generator. The fusion will give the patient significant improvement in pain and disability and improving the quality of life at 2 years.