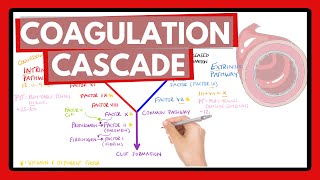
HEMOSTASIS/COAGULATION CASCADE - Intrinsic/Extrinsic/Common Pathways Amplification and Propagation
/ neuralacademy
Hemostasis is the process which causes bleeding to stop. Primary hemostasis involves the formation of a platelet plug. Secondary hemostasis involves the assembly of activated coagulation factors involved in the coagulation cascade, which converts soluble fibrinogen into insoluble fibrin strands that stabilize the aggregated platelets and define the strength of the clot. The coagulation cascade involves clotting factors, which are designated by Roman numerals (113).
The coagulation cascade has three pathways – intrinsic, extrinsic, and common. The intrinsic pathway comes into play when blood comes into contact with exposed collagen from damaged endothelial walls. Collagen is the main structural protein in the extracellular space in connective tissues. The extrinsic pathway begins when vascular tissue trauma causes blood to escape from the vascular system. It is initiated by factors external to the blood.
The intrinsic & extrinsic pathways each work towards the production of a tenase, an activating complex, which activates Factor 10. Factor 10 is part of prothrombinase, which cleaves prothrombin to form thrombin. Thrombin is an enzyme that causes the formation of a fibrin clot.
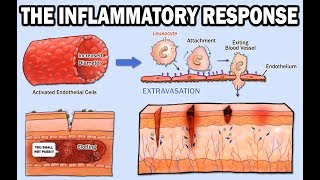
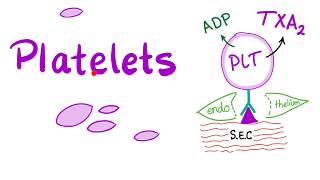
Blood vessel walls are lined by endothelial cells with antithrombic properties. However, the subendothelial layer, contains collagen, von Willebrand Factor (or VWF), and proteins involved in platelet adhesion, making it highly thrombogenic.
Platelets do not adhere to intact vascular endothelium, but stick to an injured site, recruiting and activating fellow platelets, aggregating, and aiding the coagulation cascade.
Von Willebrand Factor, or VWF When there is an injury, it binds to both collagen and to platelets, anchoring platelets to the subendothelium.
Platelet activation begins and 4 things happen:
1. Platelets undergo a morphological change
2. The platelet’s outer phospholipid membrane becomes negatively charged – which is important for the coagulation cascade to proceed. This happens thanks to scramblase, which moves negativelycharged phospholipids from the inner to the outer membrane surface
3. Platelets secrete granules
4. Platelets cause a conformational change in their GPIIB/IIIa receptor, increasing its affinity for fibrinogen. This results in aggregation
Rapid formation of a platelet plug temporarily seals off vascular injury, but this plug is not very strong. So the coagulation cascade is needed – to reinforce the blood clot with insoluble fibrin strands. The extrinsic pathway is kicked off by Tissue Factor and is the primary initiator of thrombin production.
For the tenase to form, the next critical step is activation of Factor 7. Proconvertin is activated by polyphosphates secreted by activated platelets. Tissue Factor then acts as a receptor for Factor 7a. With calcium as the activating ion, the tenase can cleave Factor 10 to convert it into the active Factor 10a.
Now, let’s look at the Intrinsic Pathway. The intrinsic tenase includes the enzyme Factor 9, or Christmas Factor, its cofactor Factor 8, or AntiHemophilic Factor, the substrate Factor 10, and calcium ions. It takes a few steps to produce Factor 9.
First, Factor 12, or Hageman Factor, is activated. Factor 12a cleaves Factor 11, or Plasma Thromboplastin, to produce Factor 11a. Factor 9, becomes an active enzyme when it is cleaved by either Factor 11a or Factor 7a.
Factor 8 circulates bound to VWF, which acts as its carrier protein. Injury activates Factor 8 and makes it separate from VWF so it can interact with Factor 9. Factor 8a is a cofactor and Factor 9a is an enzyme.
Factor 9a can convert Factor 10 to its active form with the help of its cofactor, Factor 8, in the presence of calcium ions and negativelycharged membrane phospholipids.
The common pathway, which has three goals:
1. Produce the prothrombinase complex, which converts the inactive zymogen prothrombin to the active serine protease thrombin
2. Produce a stable fibrin clot
3. Amplify the coagulation cascade
The prothrombinase complex is assembled on the negativelycharged membrane of platelets in the presence of calcium ions. Factor Xa cleaves prothrombin to form thrombin.
Thrombin cleaves fibrinogen, producing insoluble fibrin monomers that spontaneously polymerize. This polymerized fibrin is held together through noncovalent and electrostatic forces. Thrombin also activates Factor 13, a transamidating enzyme that stabilizes the fibrin by crosslinking strands.
Initially, the extrinsic pathway producing a small amount of thrombin. However, numerous positive feedback loops amplify its production. Amplification involves thrombin cleaving and activating Factor 5, Factor 8, and Factor 11, while Factor 10a activates Factor 2.
Propagation: Accumulated tenase and prothrombinase complexes on platelet surfaces results in a large burst of thrombin production. One molecule of Factor 10a leads to the formation of 1000 molecules of thrombin!