Intertrochanteric Hip Fractures - Everything You Need To Know - Dr. Nabil Ebraheim
Dr. Ebraheim’s educational animated video describes proximal femur intertrochanteric fractures and fixation.
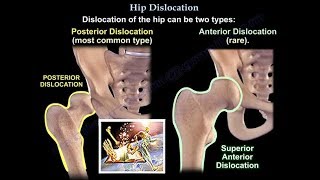
Intertrochanteric Hip Fracture occurs in the region between the greater and lesser trochanters of the proximal femur. Intertrochanteric fractures are approximately 50% of all proximal femur fractures. Fractures of the neck are about 40%. There is an important trabecular pattern of the proximal femur. Wolff’s Law is the response of the bone to stress. There is a primary tensile trabeculae and a primary compression trabeculae. There are secondary tensile and compression trabeculae. In between them is known as the Ward triangle, which is a weak area.
Deep vein thrombosis can occur in about 80% of patients. The patient will need chemical and mechanical prophylaxis. The duration and the type of prophylaxis is not determined (no unanimity). Get the patient out of bed and weight bearing as tolerated. The patient will autoregulate their ambulation.
Some patients may delay coming to the hospital. They may be on the floor for many hours or even days. Check the patient for DVT, ulcers, dehydration, and malnutrition (the patient may be very sick). May need comedical management with the medical team. Try to do surgery early (within 48 hours) because this is associated with a decreased one year mortality.
There are three types of intertrochanteric fractures; unstable, stable and reverse oblique. Regular pattern will be either stable or unstable.
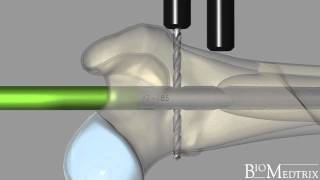
Occasionally the intertrochanteric fracture extends to the subtrochanteric area. This is considered to be a subtrochanteric fracture. The stable intertrochanteric fracture is treated with a sliding hip compression screw. The screw is inserted in the central position in both AP and lateral view within 1 cm from the joint. In the elderly patient with severe osteoporosis, it is preferred to place the screw inferiorly and posteriorly (stronger bone), definitely not anterior and superiorly. The tip apex distance should be less than 25 mm in the combined AP and lateral xrays. Tip apex distance greater than 25 mm leads to fixation failure.
In stable fractures, a two hole plate may be better than a four holed plate. This compression hip screw should not be used in reverse oblique fractures. Always look for the integrity of the lateral femoral cortex.
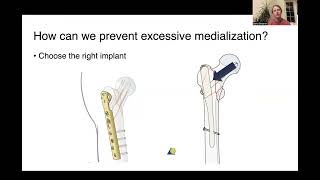
Unstable fractures are based on the loss of the integrity of the posteromedial cortex which acts as a buttress against fracture collapse. In this case, the ability of the fracture to resist compressive load is not present. The fracture could collapse into varus and retroversion. We prefer to use a rod to avoid fracture collapse and medial displacement of the fracture (rod is a percutaneous technique).
Complication of Rod fixation: fracture at the tip in short rods. Perforation of the anterior cortex in long rods due to mismatch between the bow of the femur and the bow of the rod. Also screw cut out.
Sliding compression hip screw and side plate fixation: may cause medial displacement of the femoral shaft. If you are going to use it, use it with caution.
Reverse oblique fracture is an unstable fracture pattern where the lateral cortex is not intact. Compression cannot be controlled with a sliding hip screw (due to the fractures lateral cortex). Some surgeons consider this to be a subtrochanteric fracture. May use a rod, blade plate and dynamic condylar screw, or proximal femoral locking plate. Do not use a sliding hip screw! This can lead to major displacement, nonunion and hardware failure! Fracture through the lateral cortex is a predictor for reoperation if you use the compression hip screw.
Isolated lesser trochanter fracture: avulsion in adolescence is probably due to avulsion of the iliopsoas tendon. In an older patient, rule out pathological metastatic fracture.
Implant failure occurs within the first three months. Implant failure is about 60% if the tip apex distance is more than 45 mm (tip apex distance is important). Using dynamic hip screw in reverse oblique fracture will probably fail.
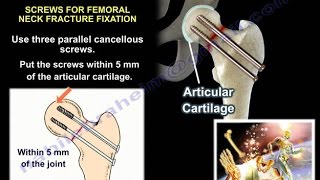
Fractures of the femoral neck and femoral shaft are missed in about 30% of cases. The fractured femoral shaft is usually comminuted, so in these cases, suspect a fracture of the femoral neck. Can get a CT scan preoperatively. Check the femoral neck by fluoroscopy before you start fixation, during fixation and after fixation. Fix the femoral neck first. Do closed reduction or open reduction if anatomic reduction cannot be obtained. Must have anatomic reduction; use cancellous screws, sometimes you may use a sliding hip compression screw. Fix the femoral shaft fracture after you fix the femoral neck fracture! may use retrograde IM rod of plate, do not use a single device to fix both fractures.
Follow me on twitter:
https://twitter.com/#!/DrEbraheim_UTMC
Donate to the University of Toledo Foundation Department of Orthopaedic Surgery Endowed Chair Fund:
https://www.utfoundation.org/foundati...