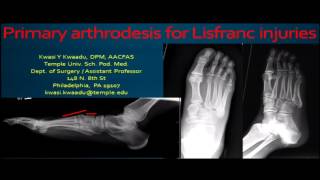
Lisfranc Dislocation Important Considerations - Everything You Need To Know - Dr. Nabil Ebraheim
Dr. Ebraheim’s educational animated video describes Lisfranc injuries of the foot.
Follow me on twitter:
https://twitter.com/#!/DrEbraheim_UTMC
Lisfranc Injuries
Lisfranc injury is a tarsometatarsal fracture dislocation that involves the medial cuneiform and the base of the second metatarsal. The injury can be purely ligamentous injury, bony injury, or a combination of both. The metatarsals are usually dislocated dorsally and laterally. The condition could be missed and may result in major disability to the patient. Some think that it is overlooked in about 20% of the time. Diastasis between the 2nd metatarsal and the medial cuneiform occurs due to rupture of the Lisfranc ligament, and this injury gives a better result if it is treated surgically. The most important ligament between the medial cuneiform and 2nd metatarsal base is the Lisfranc ligament, which is called the oblique interosseous ligament. Osseous stability is provided by the roman arch arrangement of the metatarsals. The roman arc his seen in the coronal plane, and you can see the importance of the second metatarsal. The Lisfranc ligament is between the medial cuneiform and the base of the 2nd metatarsal. The Lisfranc ligament stabilizes the 2nd metatarsal to maintain the midfoot arch. The 2nd metatarsal will fit into the mortise, which is made by the medial cuneiform and the recessed middle cuneiform (keystone configuration). The classic mechanism of Lisfranc injury is axial loading to a plantar flexed foot. Diagnosis is done by clinical examination and by xrays. The clinical signs will include plantar ecchymosis, tenderness over the Lisfranc joint, swelling on the dorsum of the foot over the Lisfranc area, and inability to walk with weight bearing. Clinically, if the patient cannot bear weight, the xray appears negative, and the patient has tenderness at the midfoot, then you do weightbearing xrays. The second metatarsal base should be aligned with the middle cuneiform at their medial borders. The fourth metatarsal base should be aligned with the cuboid bone at the medial borders in the oblique view. The dorsal and plantar aspect of the metatarsals should align with the cuneiform and the cuboid on the lateral view. Any alignment should raise the suspicion of Lisfranc injury. Diastasis between the second metatarsal and the firs metatarsal cuneiform complex more than 2mm indicates an injury to the Lisfranc joint. Look for avulsion fractures of the second metatarsal base called fleck fractures or “fleck sign”. The “fleck sign” is found at the first intermetatarsal space. Sometimes the xrays appear negative, but the clinical picture is suspicious for Lisfranc joint injury. You are going to do stress xrays. There are many ways to do stress xrays and the best way that is commonly used is weightbearing xrays compared to the other side. This will detect any occult, subtle Lisfranc injury. Sometimes you may need to do the abduction stress xray, and that may cause a dynamic shift of the metatarsals. MRI could be used for occult injuries that are not obvious in the xrays, especially after negative stress views. You may find a Lisfranc injury with a cuboid compression fracture called the “nut cracker” injury. This injury has the subtle, hidden Lisfranc injury and you have to make the diagnosis in order to treat it appropriately. For nondisplaced injury, the treatment will be nonsurgical, and it is used only when there is no displacement on weightbearing or stress views and no bony injury appears on the xrays. Follow the patient and repeat the xrays to detect any displacement of the metatarsals. Keep the patient nonweight bearing for 6 weeks. This treatment is very rare, and basically it deals with Lisfranc ligament sprains. Decide if the injury is purely ligamentous, bony injury, or mixed. If you have a purely ligamentous injury, the recommended treatment will be early fusion of the first and second tarsometatarsal joints. If you do open reduction internal fixation for purely ligamentous injury, you may have persistent pain and arthritis. The open reduction internal fixation resulted in a higher rate of the secondary surgery and a lower functional outcome. Open reduction internal fixation is not recommended for purely ligamentous injury, but if you are going to do it because you have fractures, then you need to get anatomic reduction of the injury. If the injury is purely ligamentous, then fusion is better. If the patient is treated by open reduction and internal fixation, the most common complication is post traumatic arthritis (develops in a high percentage of patients and half of these patients will go to fusion later on). If the arthritis occurs, give the patient shoe modifications, inserts, and antiinflammatory medications first, and when this fails to treat the patient, then do fusion.