Medial Epicondylitis - Everything You Need To Know - Dr. Nabil Ebraheim
Dr. Ebraheim’s educational animated video describes the condition of medial epicondylitis of the elbow.
Follow me on twitter:
https://twitter.com/#!/DrEbraheim_UTMC
Find me on Instagram @OrthoInitiative
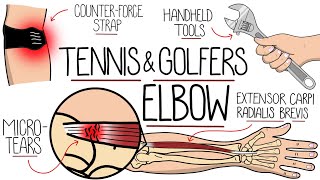
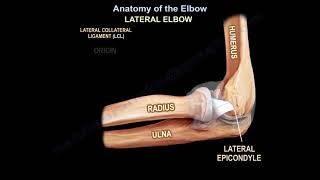
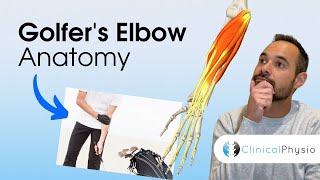
Medial epicondylitis of the elbow is also called the “golfers elbow.” It is an overuse syndrome caused by an overload of flexor/pronator mass at the medial epicondyle of the elbow. Medial epicondylitis is less common than lateral epicondylitis and it occurs more in the dominant extremity. Medial epicondylitis is common in sports and in jobs that require lifting more than 20 pounds. The medial epicondylitis affects individuals when activity involves repeated forearm pronation and wrist flexion. This will cause microtrauma to the flexor pronator group due to repeated eccentric loading to the tendon at its origin, which will involve degeneration, tendinosis and tendon disruption, angiofibroblastic hyperplasia and eventually fibrosis
The patient will have pain and tenderness around the medial epicondyles which is worse with resisted forearm pronation and wrist flexion and worse with gripping. Examined the patient for associated conditions such as valgus instability and ulnar nerve symptoms.
How do you examine for valgus instability?
Examined the valgus instability by valgus stress or moving valgus stress test.
How to examine for ulnar nerve symptoms?
Tapping on the nerve in the cubital tunnel (Tinels sign) can produce symptoms of paresthesia and pain, which is like hitting the "funny bone". You can also use elbow flexion test to diagnose for ulnar nerve symptoms, which will involve maximum flexion of the elbow with forearm pronation and wrist hyperextension for 3060 seconds.
How do you examine for medial epicondylitis?
Keep the forearm supinated and examined and will palpate the elbow epicondyle of the elbow. The other hand is placed over the volar aspect of the wrist and hand. The examiner will ask the patient to move the hand and the wrist into wrist flexion and forearm pronation while the examiner is resisting the motion and feeling the epicondyle. A positive test occurs when the patient feels pain in the medial epicondyle which the examiner is palpating. MRI is helpful. It will evaluate the associated pathology. For example: Ulnar collateral ligament injury and overhead throwers and evaluate if there is any injury to the flexor/pronator origin.
Usually you will find increased signal in T2 images that may indicate tendinosis or tendon disruption. EMG and nerve studies could evaluate the ulnar nerve compression.
Differential diagnoses
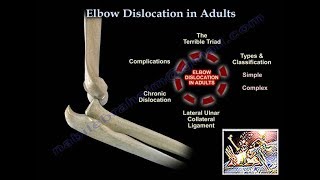
• Medial collateral injury
• Cubital tunnel syndrome
• Cervical disc herniation
• Triceps tendonitis
Treatment
• Mainly nonoperative
• Activity modification
• Rest
• Ice
• Therapy
• Counterforce bracing
• Antiinflammatory medication
The result of operative treatment of medial epicondylitis is not as good is operative treatment of lateral epicondylitis, so give the medial epicondylitis more time for conservative treatment.
Injections
You may use an ultrasound. You do not want to use multiple injections. You will do steroid injection into the common flexor tendon peritendinous area. Do not inject into the tendon, inject around the tendon. The injection will be close to the ulnar nerve, so be careful when you give the injection for medial epicondylitis. The corticosteroid injection does not have any impact on the surgical result.
Surgery
Do an open debridement and reattachment of the flexor/pronator group, especially if you try the conservative treatment for 6 months and if fails, and especially if you have the correct diagnosis. It will give a good to excellent outcome in about 85%. Most of the patients can anticipate improvement and resolution of their symptoms without surgery; however, there are some groups of patients that may need surgery. The majority of patients will go back to their prior activity after surgery without any loss of flexor/pronator strength. You may also want to do a cubital tunnel release for concomitant ulnar nerve symptoms. The worst outcome occurs when the ulnar nerve symptoms are present preoperatively. When performing ulnar nerve decompression at the elbow, the surgeon must be aware that the medial antebrachial cutaneous nerve crosses the field 3 cm distal to the medial epicondyle.
Complications
It is more difficult to treat medial epicondylitis then to treat lateral epicondylitis.
Medial antebrachial cutaneous nerve neuropathy
The nerve is in the vicinity of the incision (3 cm from the medial epicondyle).
Concomitant, moderate or severe ulnar neuropathy treated with nerve transposition leads to worse outcomes compared to no ulnar nerve pathology. It is the severity of the ulnar nerve neuropathy that correlates with the outcome of patients treated operatively for medial epicondylitis.