Sacroiliac Joint dysfunction animation - Everything You Need To Know - Dr. Nabil Ebraheim
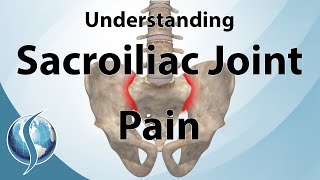
Educational video describing the important anatomic features of the sacroiliac joint and important structures surrounding
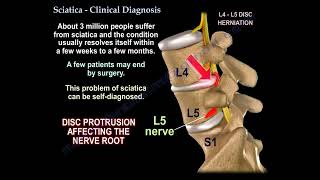
Patients that are experiencing low back pain can spend months to even years in treatment without the correct diagnosis. In low back pain, the doctors automatically link the back pain to disc conditions, even if there are no neurological findings. This is because the MRI is falsely showing protruding discs that is present in a lot of asymptomatic people. The pain itself can look like discogenic or radicular low back pain. No typical clinical history, physical examination or imaging studies that helps the clinician in making a reliable diagnosis of SI joint dysfunction. On the other hand, a successful clinical outcome of the SI joint treatment will depend on identifying the primary source of the pain, so the correct diagnosis is important.
Evaluate patient for length discrepancy, scoliosis, and the patient’s gait. Don’t forget examine patient neurologically, including the motor, the sensory and the reflexes. Examine the hip in and do the straight leg rise test, which is used to diagnose radiculopathy due to a herniated disc and its usually negative in SI joint problems. 75% or more of acute relief of the pain from the injection is diagnostic of the SI joint as the source of pain. We usually treat the patient conservatively first for four weeks before we do the SI joint injection. If the condition is chronic and the patient has no diagnosis and the pain is severe, I will do the injection early with local anesthetic steroids for diagnostic purposes.
What is the main goal of the treatment?
• Try to decrease pain
• Improve function
• Improve posture
• Lower spine and hips mechanics
Use multiple modalities including antiinflammatory medications. Antidepressants (short term), lidocaine patches, and bracing (used for a short period of time). The pelvic belt will decrease the shear forces and stress across the joint. It will limit the movement and provide relief (more helpful during pregnancy). The brace is worn at or above the greater trochanter and it can decrease the motion of the SI joint by about 30%. We treat the patient with antiinflammatory medication, with pelvic belt and physical therapy. If that does not work, then you go for the injection. If you get the result of 75% relief from the injection, then you know that the SI joint is the main source of the pain. Physical therapy will increase the flexibility, the proprioception and it will strengthen the core muscles in the pelvic region. Therapy can also include joint manipulation and joint mobilization. Injection is usually local anesthetic and steroids. We limit the injection to three injections in six months and four injections within one year. The success rate with injection within 3 months is 62%. The success rate with injection within 6 months is 58%. 2/3 of the patients have more than 50% pain reduction for 6 weeks. injection is not as good in patients with lower lumbar spine fusion. Check the patient immediately after the injection or in a day or two, but not at 6 weeks when they come to the clinic, and they tell you it did not work. You want to know if the injection worked as a diagnostic injection, then you have a diagnosis and SI fusion can be considered in the future. You also want to know if it worked as a therapeutic, and if it did work then repeat the injection in two months. Blind injection is in the SI joint only 22% of the time. The question of periarticular versus intraarticular injections, which one is more effective? Which part of the SI joint shoulder you give the injection? Using an ultrasound in overweight patient, what is the best position for injection? Is it the patient is lying down or is it when the patient is standing and bending over? Surgery is indicated in patients with positive response to SI joint injection with more than 75% relief. Done in a patient with continued or recurrent SI joint pain despite adequate conservative treatment. Percutaneous arthrodesis better than the open technique, used for revision surgery, nonunion and if the patient has an unusual anatomy. Fusion has better outcome compared to conservative management when primary pain generator is the SI joint.
The minimally invasive technique is an outpatient surgery with smaller incisions. Triangular titanium porous coated implants are the most commonly used implants and the bone grow into the implant creating a fusion. Usually, you will insert three implants (bars). The pseudoarthrosis, which means nonunion, is about 5% and when you do revision, you will probably have to do an open technique. Studies show that at one year, the CT scan shows more than 95% of bone integration into the implant on both the iliac side and on the sacral side.
The SI joint has very little motion, so the patient will not notice much of a problem from the fusion