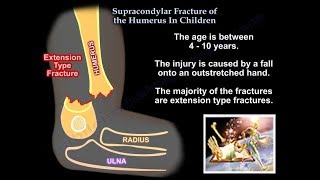
Supracondylar Fractures Of The Humerus In Children
Dr. Ebraheim’s educational animated video describing supracondylar fractures of the distal humerus in children.
Supracondylar fractures constitutes approximately 50% of all fractures.
The supracondylar region is thin and weak and thus it can fracture easily.
Fracture types:
1 Extension type:
Most common type 95%
Occurs due to falling onto an outstretched hand.
The distal fragment is displaced posteriorly.
Anterior interosseous neurapraxia is the most common nerve palsy occurring with supracondylar fractures.
Injury to the anterior interosseous nerve will lead to weakness of the flexor digitorum prefundus muscle to the index finger, and the flexor pollicis longus muscle.
The patient will not be able to do the OK sign or bend the tip of his index finger.
Radial nerve neurapraxia is the second most common palsy and is evident by weakness of the wrist and fingers extension.
2 Flexion type:
It is rare and occurs due to falling directly on a flexed elbow.
The distal fragment is displaced anteriorly.
This type of fracture may be accompanied with ulnar nerve neurapraxia.
Injury to the ulnar nerve will lead to loss of sensation along the little finger.
Later on, the patient may have weakness of the intrinsic hand muscles and clawing.
Gartland classification system:
Type I: Nondisplaced
Type II: Angulated with an intact posterior cortex
Type III: Completely displaced
Type IV: Complete periosteal disruption, and shows instability in flexion and extension.
Radiology:
Plain AP and lateral xrays should ne obtained.
A posterior fat pad sign seen on a lateral view xray should increase your suspicion of an occult fracture around the elbow.
The anterior humeral line:
• On a lateral view xray, the anterior humeral line is drawn along the anterior border of the distal humerus.
• Normally, the anterior humeral line should run through the middle third of the capitellum.
• In extension type fractures the capitellum will be displaced posteriorly relative to the anterior humeral ling.
Baumann’s angel:
• Is formed by a line perpendicular to the axis of the humerus and a line going through the physis of the capitellum.
• normally, baumann’s angle should measure at least 11°.
Examination:
on examination it is very important to assess the neurovascular structures.
The anterior interosseous nerve is assessed by asking the patient to do the OK sign with his hand.
The radial nerve is assessed by asking the patient to extend the wrist and the fingers.
The ulnar nerve is initially assessed by loss of sensation along the little finger; later on the patient may have weakness of the intrinsic hand muscles and clawing.
Treatment:
Nonoperative treatment:
• Indicated for type I fracture.
• Usually consists of splinting or casting the elbow for duration of 34 weeks.
• It is very important to remember not to flex the elbow on the splint or cast more than 90° in order to avoid vascular compromise and compartment syndrome.
Operative treatment:
• Type II and type III fractures are usually treated by closed reduction and percutaneous pinning.
• During reduction, pronation of the forearm during elbow flexion helps correcting a varus deformity.
After reduction check for a gap in the fracture.
The neurovascular bundle may be trapped there.
Free the brachialis muscle from the fracture site if it is interapositioned there.
Fixation is usually achieved with 23 divergent lateral pins, depending on stability.
Medial pins can also be added depending on the stability.
Open reduction is indicated only when closed techniques are unable to achieve appropriate reduction of the fracture.
Avoid posterior dissection to preserve vascularity of the fractured segment.
Fracture reduction and fixation should be done emergently in cases of vascular compromise.
Complications:
Neurapraxia (ususally resolve and is thus observed).
Cubitus varus deformity occurs due to malunion of the fracture.
It only presents a cosmetic problem since it does not affect function.
This deformity can be corrected later on by supracondylar valgus osteotomy.
Vascular problems such as compartment syndrome.
Volkmann’s ischemic contracture:
• Occurs due to compression of the brachial artery when the patient is placed in a cast in hyperflexion (more than 90°).
Important scenarios:
Patient may present with a displaced type III fracture, and he has a pulseless hand.
1 He may have adequate circulation which is evident by a normal temperature and color of the hand.
2 Or he may have inadequate circulation, which is evident by a blue and cold hand.
In both cases, urgent closed reduction and percutaneous pinning is required.
After closed reduction and percutaneous pinning:
1 if the circulation is adequate: observe the patient and place in a splint that is 45°.
2 If the circulation is inadequate: the patient will require vascular exploration and repair.